If you’ve been told that you need a hysterectomy, you may feel scared and unsure of what to expect. If you’re preparing to get a hysterectomy and feeling worried, the first step is to take a few deep breaths. Here we go through everything you need to know about the hysterectomy procedure and hysterectomy recovery. Being equipped with knowledge is key to a smooth recovery process to get you back to feeling like yourself as quickly as possible.
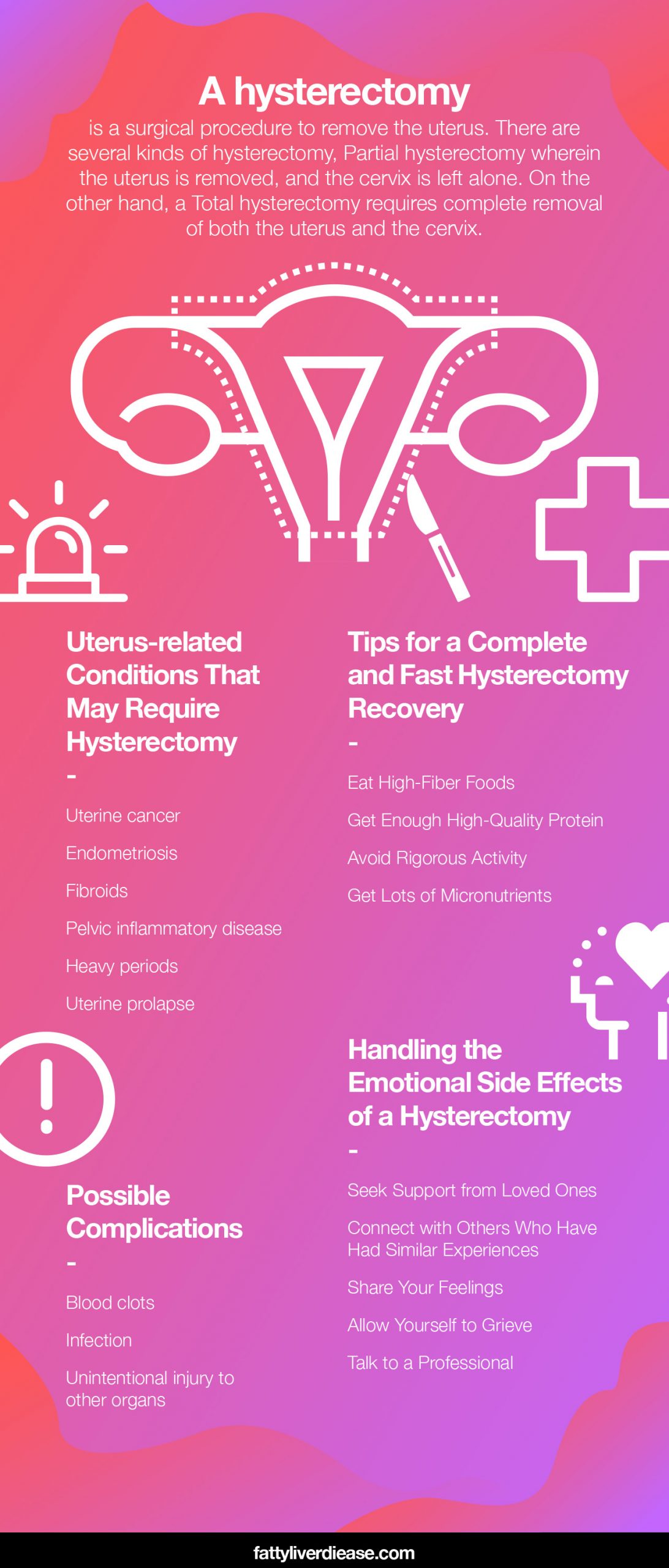
What Is a Hysterectomy?
A woman may undergo a hysterectomy to remove the uterus. It is much more common to undergo a hysterectomy after childbearing years since the uterus is required to house a growing fetus as it develops.
There are also a couple of different kinds of hysterectomy surgeries. A woman may undergo a partial hysterectomy, which means that the uterus is removed, and the cervix is left alone. On the other hand, a total hysterectomy requires the complete removal of both the uterus and the cervix.
So, why might a woman need to undergo a hysterectomy? There are a number of situations that may prompt a doctor to recommend getting a hysterectomy. There are several uterus-related conditions that affect women’s health and may require a hysterectomy.
- Uterine cancer: If cancerous growths develop in the uterus, it may make the most sense to remove the uterus to prevent metastasis to other organ systems.
- Endometriosis: Endometriosis is a common cause of hysterectomy recommendations. Endometriosis is a condition in which endometrial tissue grows outside of the uterus and bleeds every month during menstruation. Endometriosis varies in severity, but it can be extremely painful and uncomfortable. after childbearing years if endometriosis worsens or becomes unbearable, it might be a good idea to get a hysterectomy. However, keep in mind there are some instances when getting a hysterectomy doesn’t completely resolve endometriosis. Talking to your physician will help you weigh the pros and cons of undergoing the surgery.
- Fibroids: In contrast to cancer, fibroids are small benign growths on the uterus. Though they are not cancerous or harmful, they may cause irritation and pain that impacts quality of life. As a result, it may make sense to have the uterus removed.
- Pelvic inflammatory disease: Pelvic inflammatory disease may develop as the result of an untreated bacterial infection. If bacteria grow and multiply in the uterus, uterine tissues become irritated and inflamed, causing scarring and pelvic pain. If a woman is past childbearing years and has developed a severe case of pelvic inflammatory disease, it may make sense to remove the uterus.
- Heavy periods: Simply having extremely uncomfortable periods, even in the absence of underlying conditions, may be sufficient to qualify you for a hysterectomy.
- Uterine prolapse: As the body ages, tendons and connective tissue begin to weaken over time. If the tendons and connective tissue around the uterus and abdominal area get too weak, the uterus may begin to collapse or move downwards in the abdominal cavity. This descent of the uterus can interfere with normal urinary function and the ability to pass bowel movements. It can also cause pelvic pain that interferes with quality of life. Most women struggling with pelvic pain are older and past childbearing years, which means that getting a hysterectomy may be the best solution.
How Is a Hysterectomy Conducted?
There are several surgical strategies for conducting a hysterectomy. A hysterectomy can be performed laparoscopically, vaginally, or through open surgery. Most of the time, the method of surgery depends on your specific needs.
For example, if you are also suffering from a condition that affects the ovaries and fallopian tubes, a surgeon may elect to perform an open abdominal hysterectomy in order to more easily perform a hysterectomy while also removing the ovaries (called an oophorectomy) and fallopian tubes, if needed
In the case of a laparoscopic hysterectomy, the surgeon will use minimally invasive techniques. To conduct this kind of hysterectomy, a small incision will be made in the abdominal area. A slender tool called a laparoscope, which has a tiny camera attached to it will be inserted through the incision to allow the surgeon to both see the internal organs and conduct the surgery.
Who Performs a Hysterectomy?
To first determine whether or not you need a hysterectomy, you will consult your obstetrician/gynecologist (also called an OB-GYN). These physicians are specialists in gynecology, which is the study of the female reproductive system. Many OB-GYNs also perform surgeries, though some instances may require a general surgeon to perform your procedure.
What to Expect During a Hysterectomy Procedure
If you are currently scheduled for a hysterectomy, it’s helpful to know what to expect during the procedure. Prior to surgery, your physician or surgeon will perform a pre-surgery examination to make sure that your body is fit and healthy enough to undergo surgery and be under anesthesia. The doctor will perform a physical examination as well as a blood test to make sure that all organs are functioning as they should. In many cases, an EKG may also be performed to assess heart function.
You will probably also be instructed to avoid solid foods for about 12 hours prior to the surgery and to take a shower at home with anti-bacterial soap, before coming to the hospital.
When in the hospital, a nurse will assess your vitals and prepare you for the procedure. Your anesthesiologist will also speak to you before the procedure to answer any questions and to make sure you’re feeling comfortable about the sedation during the procedure. Your surgeon will also speak to you before the surgery to answer any questions and make sure you understand the surgery.
The procedure usually requires about two hours in the operating room, followed by a hospital stay of one or two days to monitor your progress. After a couple of days, you will be discharged from the hospital to continue your recovery at home.
The longest part of the hysterectomy procedure is the recovery process following the actual surgery.
What to Expect During Hysterectomy Recovery
Following recovery, it is normal to feel tired and weaker than usual. It’s also common to feel like you’re not quite as hungry as usual. It’s also normal to observe vaginal bleeding in the aftermath of the surgery, as your body heals. You will likely also experience pain in the lower abdomen. Your physician or surgeon will prescribe a regimen of pain medications to help manage the pain as you heal.
How long does it take to recover from a hysterectomy? Hysterectomy recovery time may vary from a few weeks to a couple of months, depending on whether you also need other surgical procedures.
When to Seek Medical Attention
Though healing from every surgery is notoriously not a fun process, it’s important to know when symptoms have progressed from normal to serious. If you are experiencing fever, chills, oozing of the surgical site, extreme abdominal pain, unusual vaginal discharge that concerns you, or heavy vaginal bleeding that does not resolve, it’s a good idea to seek medical attention immediately. Severe chest pain and trouble breathing are also signs of a complication and you should seek emergency medical attention.
Tips for a Complete and Fast Hysterectomy Recovery
Abdominal, vaginal, and laparoscopic hysterectomy recovery all benefit from the same strategies to promote healing. To heal as quickly as possible and get back to the activities you enjoy, it’s important to prioritize your recovery and take care of your health. Here are some tips for making your recovery as fast and painless as possible.
1. Eat High-Fiber Foods
High-fiber foods are your friends when recovering from a hysterectomy. Getting either a vaginal hysterectomy, laparoscopic hysterectomy, or open hysterectomy all interferes with the normal functions of the abdominal organs. When the abdominal area is operated on, the organ systems in proximity often dial-down activity, to promote healing of the directly affected area. The digestive system is the primary organ system that is indirectly affected by any abdominal surgery.
As a result, ileus develops, which means that the digestive system is frozen in a sense. Digestion is significantly slowed down and passing bowel movements becomes extremely difficult. Ileus can be effectively combatted by eating foods that are packed with insoluble and/or soluble fiber. Fiber is critical to facilitating the movement of foods through the digestive system and stimulating regular bowel movements. If high-fiber foods do not help produce a bowel movement within 5-7 days, it’s important to speak with your doctor. He or she may prescribe a laxative to help get your digestive system moving.
2. Get Enough High-Quality Protein
Eating enough protein is one of the most important dietary steps you can take when recovering from a hysterectomy. Protein provides the raw materials that your body requires to heal from surgery. The building blocks of protein are amino acids. Essential amino acids, specifically, promote healthy immune system function. The essential amino acids are also vital for repairing tissues following an injury or surgical intervention. Beyond simply getting essential amino acids in your diet, getting optimal ratios of these essential amino acids is important to support repair.
So, how can you get optimal ratios of essential amino acids on a daily basis? Certain protein sources contain ideal ratios that the body needs. Make sure you get high-quality animal proteins. The best animal-based protein sources include low-fat milk, cheese, yogurt, lean meats, and fish.
If you’re a vegetarian or vegan, don’t worry. You can still get all the essential amino acids you need to recovery quickly. To get optimal ratios of essential amino acids from plant-based sources, it’s important to consume several plant-based sources of protein throughout the day. For example, eating ground flaxseeds, brown rice, almonds, and tofu over the course of the day would ensure that you have the essential amino acids to recover efficiently from a hysterectomy.
Plus, since physical activity will be restricted as you recover from a hysterectomy, getting plenty of essential amino acids is critical for making sure that you don’t lose muscle mass throughout your recovery. Muscle atrophy is particularly concerning for older adults, whose muscle wastes at a faster rate. For older adults, muscle wasting can lead to weakness and an increased risk of injury.
If you’re not feeling hungry after surgery, getting all the essential amino acids your body needs can sometimes be tricky. If this is the case, try adding a high-quality essential amino acid supplement to your diet. You can easily add essential amino acid powder to any food or beverage that you’d like, such as water, oatmeal, soups, and smoothies.
3. Avoid Rigorous Activity
Though walking and moving around is encouraged as you are able, engaging in rigorous activity may jeopardize the physical healing after your hysterectomy. It’s best to avoid intense activities like heavy lifting, running, and anything that may pull at stitches or cause stress to any internal organs. You may even be instructed to take time off from work, especially if your job is based on physical activity or manual labor.
4. Get Lots of Micronutrients
While macronutrients supply energy, micronutrients afford lots of vitamins, minerals, and antioxidants that help your cells and organ systems operate as efficiently and smoothly as possible. Effectively-operating organ systems are particularly important as you recover from surgery.
Handling the Emotional Side Effects of a Hysterectomy
For many women, undergoing a hysterectomy is accompanied by significant emotional impacts. Many women feel a sense of loss after one or more reproductive organs have been removed. A woman may feel that part of what has made her a woman has been taken away.
It’s important to understand that this is a completely normal and natural way to feel. Taking steps to support and protect your emotional health as you recover from a hysterectomy is equally crucial to supporting your physical recovery.
Here are a few tips for supporting your mental health as you recover from a hysterectomy.
1. Seek Support from Loved Ones
Loved ones can provide immense support – both physically and mentally – as you recover from your hysterectomy procedure. Make sure that you arrange to have friends and family help transport you to and from the hospital, both before and after your procedure. You may want to ask loved ones to have some prepared meals in the refrigerator and ensure that your cupboard is stocked with food. Even having a friend or family member come over and watch TV or watch a movie with you can be comforting and calming as you recover.
2. Connect with Others Who Have Had Similar Experiences
Connecting with others who have also gotten a hysterectomy can be extremely comforting. You may even find that there are online or in-person support groups that help women come together to discuss common experiences like getting a hysterectomy. Talking to others about their experiences and coping strategies can help provide you with a toolkit of strategies to help lessen your emotional burden. Plus, relating to others who’ve dealt with similar situations is extremely comforting, helps you feel less alone, and helps reveal a light at the end of the tunnel.
3. Share Your Feelings
One of the least productive things you can do when suffering from loss is to stuff your feelings and keep them to yourself. When we do this, feelings tend to linger and fester, becoming even stronger until they explode at some point down the road. Instead, acknowledge any feelings you may be experiencing. These feelings may include shame, guilt, sadness, and loss. Every woman is different, and the grieving process may look a little different for each one. However, in any case, reaching out to someone you trust and sharing your feelings will help take the pressure off of yourself.
4. Allow Yourself to Grieve
The sense of loss following a hysterectomy is real. Allowing yourself the time and space to grieve and process your feelings will ultimately lead to more complete emotional healing. Don’t feel guilty for being sad. Simply allow yourself to experience your feelings, and it will make it easier to move on.
5. Talk to a Professional
For many women, having a hysterectomy can be a traumatic experience. Talking to a mental health professional is very helpful, especially if you’re having lingering, severe despair following your hysterectomy. Psychologists and counselors can help you work out your feelings while providing helpful coping strategies, and they are particularly skilled in dealing with lingering trauma and depression. It’s important to know that there are options for handling your feelings, and you don’t need to feel like this forever.
Possible Hysterectomy Complications
What are the negative side effects of hysterectomy surgery? As with any surgery, there are risks and complications that may occur, even though most are rare.
- Blood clots: Blood clots are a risk factor in undergoing any kind of surgery. Undergoing surgery increases the risk of experiencing blood clots because both during and after the surgery, you often experienced prolonged periods of immobility. While in the operating room, the surgeon or medical assistants will put wraps on your lower legs that administer massage and keep the blood circulating. Upon leaving the operating room, however, you will need to get your blood moving manually.
- Infection: Infection is a possible complication, as is the case with any surgery. The risk of infection tends to be a bit higher with open surgeries since open procedures expose more internal tissues to the open air. Antibiotics may be prescribed as a preventative measure.
- Unintentional injury to other organs: Though this kind of complication is rare, it is possible that other internal organs in the abdomen may be injured while the uterus is surgically removed. If this is the case, you may require further surgery to repair any damage.
Down the Road: What to Expect from a Hysterectomy
A hysterectomy can relieve you from many unpleasant symptoms associated with conditions like pelvic inflammatory disease, endometriosis, uterine cancer, uterine prolapse, and fibroids. After recovery, you will likely experience a dramatic increase in quality of life and the ability to engage in the activities you enjoy.
Many women wonder if they will still experience hormonal fluctuations and conditions associated with hormonal changes, such as menopause. If you have undergone a hysterectomy but the ovaries have been left in place, you will still experience hormonal changes and associated symptoms like hot flashes, mood swings, insomnia, and vaginal dryness. It’s important to talk to your doctor about ways to mitigate your menopausal symptoms, including hormone replacement therapy and other options.
Conclusion
Though a hysterectomy is an invasive surgery that requires ample recovery time both physically and emotionally, there are steps you can take to expedite the healing process and ensure that you make a successful recovery. Eating a healthy diet, drinking plenty of fluids, and taking care of your mental health will help make sure you return to your normal activities as soon as possible.